Pandemic and Pandemonium

It’s only March and 2020 already feels like a really long year. Like many around the world, every waking moment is filled with news of COVID19. As the SARS-CoV2 virus steadily continues its march across countries and continents with no respect for borders, it leaves panic and fear in its wake. As an infectious disease physician and a virologist, I try to be the voice of calm, holding on to the science of what we know about epidemics and this pandemic so far – “this too shall pass” has become a mantra I repeat to myself and loved ones seeking reassurance. As a human with parents in the most vulnerable age bracket being rational is much harder.
Mama Said Not to Worry

You see my parents are not only over age 60, they also reside in sub-Saharan Africa which is home to the world’s most vulnerable health systems. I called my mother earlier this week to check in and reinforce the messaging on infection prevention strategies and social distancing. It is the peak of the dry season in Cameroon, and like in many parts of the continent this means sweltering heat and scorching temperatures through the day. My mother knows my choice of specialty has me at the frontlines of this pandemic in the USA where I work. She tries to be reassuring “Don’t worry about us Bo, we are being safe, I don’t think the virus can even survive this horrible heat” she says. We both laugh nervously at this and chat about how so far, Africa seems to be relatively spared from a severe outbreak. I tell her to continue being safe and promise to check in again later in the week.
Hoping for the best

Africa so far has been relatively spared a severe outbreak on the scale of which we have seen in parts of Asia and now in parts of Europe and the United States. As of March 13th, there were 147 confirmed cases of COVID19 in 15 African countries (most of these imported from Europe and Asia) with 4 deaths and very limited evidence of widespread community dissemination. Many have pondered the reasons behind this. I do believe that there is some merit to what I am calling “Mama’s dry season theory” but I think this only partially explains why Africa hopefully might actually sit this one out (i.e. be spared a catastrophic outbreak).
Climate Matters

Many have expressed the hope that as the temperatures rise in temperate regions this could actually limit the spread of the virus and eventually lead to a sharp decline in cases. The evidence from other respiratory viruses like influenza which peak in the winter and decline in summer suggest that this may actually hold true to a certain degree. With hotter temperatures infectious droplets which transport the virus particles are likely to dry up more quickly and not travel as far. Ultraviolet rays from more sunshine in spring and summer months will make it more difficult for the virus to survive for extended times in the environment. Also, people will spend more time outdoors thus limiting indoor crowding.

The influenza surveillance data for countries in sub-Saharan Africa, albeit limited, consistently show lower detection of circulating Influenza A and B. This may be in part be due to the fact that the climate is less favorable to the sustained transmission and persistence of viruses which predominantly spread through droplets. Other human coronaviruses have behaved similarly, showing seasonality and a predominance in the winter months but only time will tell whether SARS-CoV will follow this pattern.
Age Really Matters

So far what we have seen in the COVID19 pandemic are very high rates of severe illness and death in patients older than 60 years and with underlying chronic medical conditions. The young and healthy have generally done well, with zero deaths in the 0-10-year age group and < 2% of deaths in people under the age of 30. Africa is the second largest and second most populated continent on the planet after Asia. Its population as a whole is very young with 60% of the entire continent aged below 25! This makes it by far the youngest continent in the world. In Italy which has the worst COVID19 outbreak outside of Asia, the median age is 47.3 years. Compare this to the 17.9 median age of Africa’s most populated nation Nigeria and the difference is striking.
If and when community spread becomes established in sub-Saharan Africa, I believe that herd immunity will accumulate quickly in a youthful population which is more likely to have mild disease and a higher rates of recovery and survival. This will be crucial in providing some degree of protection to continent’s elderly (> 60 years old), who represent 35% of the population . Another factor worth mentioning is that many of the Africa’s elderly live out their latter years within the family unit and nursing homes for the elderly are not the norm as in most developed countries. This limits the threat of high lethality outbreaks in settings with concentrations of vulnerable persons.
Limited Mobility… A Saving Grace?

The African continent by its sheer size and limited access to good road and rail networks is not as well connected as Europe, the United States and or Asia. Air travel is only marginally better with very few flight options between countries and associated significant cost of air travel as a result. Even within the borders of individual countries, travel between regions in a country is often limited by challenging terrains and unsafe roads. These logistical challenges which severely limit movement within the continent, may in the face of this pandemic be a positive factor for slowing the spread of COVID19 between countries. Whether this will have a significant role in how widely the virus will spread within the continent is something that cannot be predicted at this time and only time will tell.
What about Immunity?

Another question which has frequently come up in conversations with friends and family is whether being black and of African descent is protective against infection with SARS-CoV2. The simple answer is no, it is not. While we have fewer cases in Africa so far due to the reasons detailed above there is no evidence at this time to suggest that race or ethnicity confers a special protective benefit against COVID19. With that being said, the high burden of parasitic infections in sub-Saharan Africa has been suggested as protective in reducing the severity of some viral infections.
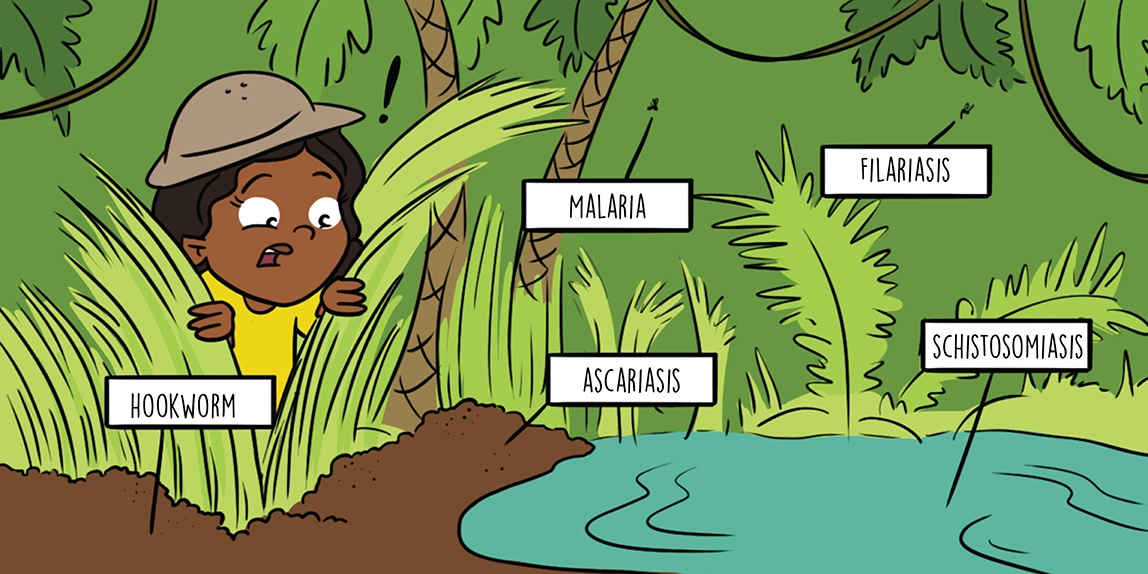
Good examples of this phenomenon are reduced severity of diarrhea from rotavirus infections in children who also concomitantly have infection with the intestinal parasite Giardia lamblia. A similar effect of decreased severity of Chikungunya virus infections has been noted with concomitant plasmodium infection. The immune mechanisms which explain these observations are complex and incompletely understood and also well beyond the scope of our current discussion (further reading in this link). Whether the phenomenon of parasitic antagonism will have an impact on severity COVID19 in Africa remains to be determined, but is certainly an interesting thought.

Coronaviruses are widespread among mammals and birds and cause a variety of diseases. Human coronaviruses are major causes of the “common cold” and generally cause mild infections. Occasionally, animal coronaviruses successfully emerge and adapt to infect humans as we have seen with SARS, MERS and now SARS-CoV2. Whether frequent exposure to animal coronaviruses through manipulation for food or close contact with animals and birds will confer any meaningful cross-protection against COVID19 in Africa is unlikely, as this has not been observed in other parts of the world. Data from patients who survive infection with SARS-CoV and MERS-CoV suggest that those who recover from these infections develop some degree of humoral immunity which can last for 2-6 years and we hope this will be similar for SARS-CoV2.
Getting better but not there yet

Earlier this week I took care of my first patient with confirmed COVID19. I know there will be many more in coming days and weeks. Things now feel very real with China and Italy clearly illustrating how much pressure a flood of cases can inflict and even break the most robust healthcare systems. The fragile healthcare systems in Africa do not stand a a fighting chance to cope with the clinical care of a large volume of patients. The lack of ventilators, limited numbers of ICU beds, and severe short-staffing in medical personnel are not challenges which can be overcome overnight. This makes aggressive public health measures to prevent community spread from establishing itself absolutely key. Basic hygiene remains a big challenge in many parts of the continent where access to soap and clean water are not always a given.

The continent may draw some level of comfort from the points I have discussed above. However, we cannot afford to be complacent. Following common sense public health measures of social distancing and effective hand hygiene remain crucial in slowing/delaying community spread. Local governments will need to double their efforts to ensure that when they call for more hand washing and social distancing, they are also putting their populations in the position to adhere to these measures.

One of the positives that emerged from the Ebola outbreak in W. Africa in 2016, is countries stepping up their public health response preparedness by improving laboratory capacity, strengthening public health institutions and increasing outbreak surveillance systems. There’s still a lot that needs to be done but these changes represent the first steps in the right direction. As we nervously continue to watch the numbers of COVID19 cases, we can only hope that Africa will be spared the worst. This year, the continent has already dealt with several outbreaks including measles, cholera, monkey pox, Lassa fever and Ebola with several still ongoing.
#ThisTooShallPass
The current pandemic of COVID19 illustrates more than ever before, the need to respond and prepare for outbreaks as a global collective. We have to do better at ensuring that the weakest links in the chain can respond and stop any outbreak from becoming a pandemic. This will not happen if every country continues to only look within its borders and we wait for pandemics to happen before we react. The reactionary response is much more costly than planning ahead and hopefully the lessons will stick this time. Three and a half months ago Wuhan and Hubei provinces in China seemed like very far off places. I occasionally spared a thought for medical colleagues at the frontlines there fighting the spread of the virus and wondered what it was like to be in their shoes.

Today alongside valiant co-workers, I find myself on America’s frontline while worrying about my parents in Cameroon. Things now feel uncomfortably close to home on all fronts. Mama’s always right they say and I sure hope her “dry season theory” holds true . While we await the warmer temperatures let’s remember to be kind to one another, provide a word of encouragement if you see someone who is struggling at this time. We will need each other more than ever in the coming months but I promise you we will get through this. #ThisTooShallPass.
Written by : Boghuma . K. Titanji






