Vaccines in the News…Again
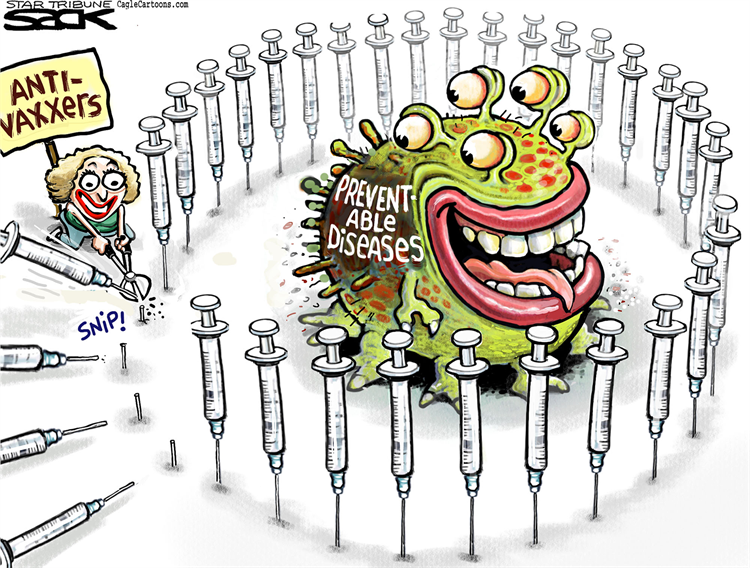
The start of the year has been dominated by news headlines of ongoing measles outbreaks in the United States and Europe. Antivaxxers seem to be winning the messaging on vaccination by convincing a growing number of parents to decline vaccinating their children. This is very concerning to public health experts who worry about more frequent outbreaks and deaths from preventable childhood diseases.
Wealthy countries, fortunately do not have to contend with the additional issues around sustained supply and access to life-saving vaccines for those who actually want them. In less privileged countries, the main barrier to vaccination remains the lack of continued access and stable supplies, a constant challenge for health authorities .
In November 2018, the pharmaceutical company Merck announced it was pulling out from its agreement with GAVI – the vaccine alliance, to supply its rotavirus vaccine Rotateq® to four low income countries in West Africa. This announcement at face value sounds like another boring headline. It however has implications that run deep, but hardly created a ripple in the constant stream of news.
More Than Just Diarrhea

The WHO estimates that worldwide there are 1.7 billion cases every year of diarrheal illnesses in children under 5. That’s a lot of poo, but more importantly these diseases kill half a million children every year. For those who survive through childhood, there is significant morbidity including malnutrition, growth retardation, recurrent infections and impaired cognitive development. A large proportion of affected children live in low- and middle-income countries, with obvious implications for the economic development and population growth of these regions. Rota virus infection is the leading cause of diarrhea-illness in early childhood and kills about 215,000 children under the age of 5 every year.
The development of two effective rotavirus vaccines administered orally has been a saving grace for many children in developing countries especially in Africa. Following successful clinical trials demonstrating their efficacy in poor and high mortality settings, the WHO recommended the inclusion of these vaccines in the national immunization programs of all countries.
A Worthy Investment?
Rolling out Rotavirus vaccination in high mortality regions has been challenging but is a worthy investment with indisputable positive outcomes. Since its introduction in Ethiopia in 2013, Rotavirus vaccination has saved an estimated 3700 childhood lives and 800,000$ in household expenditures every year. Even more striking is the projection that expanding its use to all eligible countries could prevent an estimated 180,000 deaths and avert 6 million hospital and clinic visits, saving 68 million dollars in annual costs. With numbers like these, funding this vaccine should be a no brainer and a guaranteed win for all parties involved.
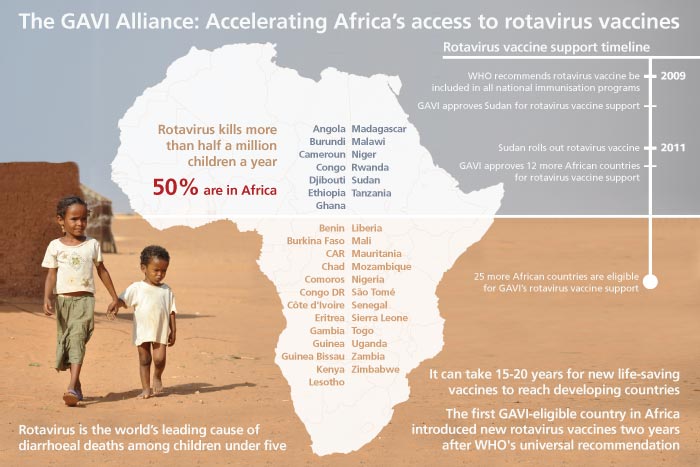
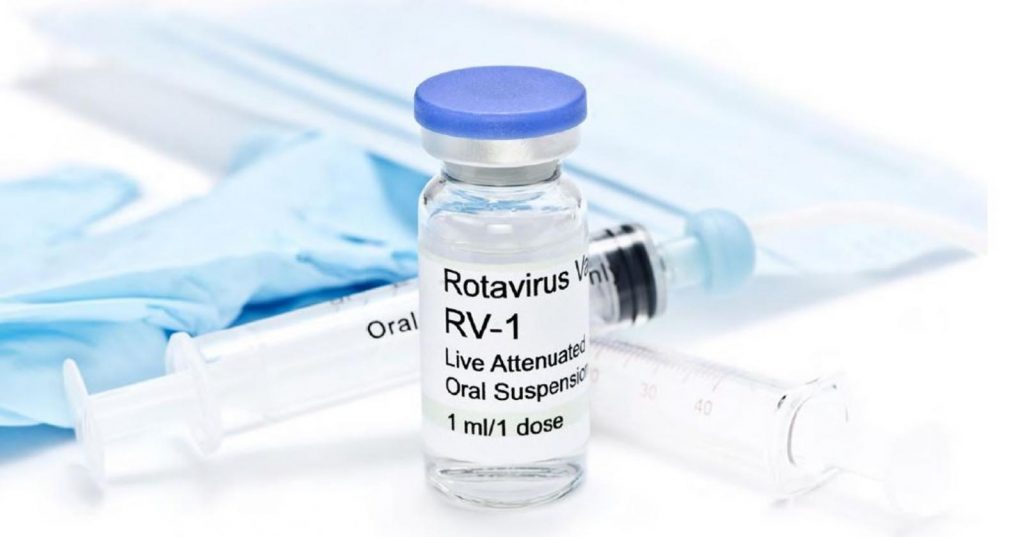
There are two main licensed Rotavirus vaccines on the global market today, Rotarix® manufactured by GlaxoSmithKline and Rotateq® manufactured by Merck and Co. A lot of the countries in sub-Saharan Africa have only been able to afford these vaccines with the support of the GAVI. In 2011, Merck agreed to sell Rotateq® to GAVI at a discounted price of 3.50$ per dose. Through this agreement over the past 6 years, 30 million doses of the vaccine have been delivered to four countries in West Africa – Burkina Faso, Ivory Coast, Mali and Sao Tome and Principe. GSK also sells its Rotavirus vaccine Rotarix, to GAVI at a reduced cost of 2.25$ per dose and has so far delivered 220 million doses to 42 countries around the world through this agreement.
A Change of Heart with Serious Implications
All seemed to be going well until the end of 2018 when Merck informed GAVI it was backing out of the agreement and will not deliver a third of vaccine doses needed for 2018 and 2019. They also plan to cease all rotavirus vaccine deliveries to these countries by 2020. This casual change of heart by Merck, in reality leaves 2.5 million vulnerable children without an alternative Rota virus vaccine source in just three years.

Merck has cited “country-specific requirements, unanticipated manufacturing issues and packaging challenges that put greater stress on our already strained packaging capacity” as the main reason for pulling out of the supply agreement. Simultaneously, however it is moving to start supplying the same vaccine to China at a higher price of 40$ a dose. The higher profit margin, promised by the more lucrative Chinese markets sticks out like a sore thumb and makes Merck’s supply chain excuse a little less plausible.
Too hard to resist – The lure of the Chinese vaccine market
China’s vaccine market is sizable but also notoriously difficult to break into for multinational BigPharma companies. Until very recently, the Chinese government required that all vaccines be tested in clinical trials conducted within the country, prior to their introduction. As a result, a lot of the vaccines used in the country are manufactured by local Chinese pharmaceutical companies. Recent scandals around the distribution of faulty vaccines by major Chinese pharmaceutical companies has created vaccine shortages and a loss of trust in locally manufactured vaccines. This has led to the relaxation of some of the regulations around vaccine supplies and opened a window for foreign pharmaceutical companies to come in.

With an estimated 17 million births every year, gaining authorization to sell vaccines on the Chinese market can mean a significant profit boon for any pharmaceutical company. When GSK gained approval for its HPV vaccine to be sold in China, this boosted global sales by approximately 60 percent to $185 million, a windfall of profit for the company. Merck has also had success on the Chinese markets with their own HPV vaccine. They saw a 24% boost in sales, an estimated $660million in the first quarter of 2018 following its introduction in China.
Rotavirus infection remains a big problem in China where it kills an estimated 3000 children every year and causes 30-40 percent of hospitalizations and doctor visits. Although no one can predict how well Merck’s Rotateq® will compete with the locally manufactured Rotavirus vaccine currently available in China, the potential for the company to make a larger profit margin in the Chinese market is undeniable and certainly worth the effort. Sadly, this likely means diverting supply chain resources from the commitments made to four West African countries in the pursuit of these bigger profits.
Protecting all children – Beyond Profits

One could argue that the four African countries left in limbo by Merck, could simply switch to the GSK Rotarix® vaccine as an alternative. In reality, the logistics around switching a vaccine supplier in developing countries, requires several years of pre-planning and costs agreements which are challenging to put in place given the timeframe.
Furthermore, GSK does not plan to expand its supply agreements for its Rota vaccine beyond the countries it currently covers. Two new Rotavirus vaccines produced by Indian, pharmaceutical companies have been recently pre-qualified by the WHO to be sold at affordable costs to GAVI. Rolling them out on a large scale could take several years and will not reliably close the supply gap that Merck leaves behind in the short term.

All children need reliable access to life saving vaccines. No monetary value can be substituted for a life saved by effective vaccination, be it that of a Chinese child or an African child. Merck’s decision on discontinuing their supply of rotavirus vaccines to four West African countries, sets a dangerous precedent. It also highlights the precarity that many developing countries continue to face when it comes to the supply of life saving vaccines and medicines.
Beyond profits and lucrative markets, the focus should be on every s child having access to vaccines regardless of whether they come from a poor or a wealthy country. Even a year’s lapse in supply puts millions of innocent babies at risk of death – an unjustifiable failure, which places an entire generation in peril.
Written by Boghuma K Titanji




















 The odds are incredibly harsh for patients like Jay for whom a diagnosis of HIV at some point in their lives almost seems to be an inevitable outcome. The reasons behind this raging epidemic are multifaceted and extremely complex
The odds are incredibly harsh for patients like Jay for whom a diagnosis of HIV at some point in their lives almost seems to be an inevitable outcome. The reasons behind this raging epidemic are multifaceted and extremely complex  white gay men very quickly became the face of the epidemic due to the sheer numbers of them who were infected and dying from AIDS.
white gay men very quickly became the face of the epidemic due to the sheer numbers of them who were infected and dying from AIDS.  The advent of the HIV epidemic in the black MSM community, joined the ranks of existing healthcare disparities which disproportionately affect minorities in the United States and the extensive stigma and discrimination associated with being black and MSM.
The advent of the HIV epidemic in the black MSM community, joined the ranks of existing healthcare disparities which disproportionately affect minorities in the United States and the extensive stigma and discrimination associated with being black and MSM. When infections do occur, access to healthcare services is hindered by a lack of education on available options for prevention, testing and treatment, homelessness and poverty, substance abuse issues and the stigma of being labelled as infected with HIV.
When infections do occur, access to healthcare services is hindered by a lack of education on available options for prevention, testing and treatment, homelessness and poverty, substance abuse issues and the stigma of being labelled as infected with HIV.  As we mark yet again another world AIDS day this December 1st, there are many reasons to feel hopeful about how far we have come since the beginning of the HIV/AIDS epidemic. We have effective treatments that allow people infected with HIV to live normal lives and have essentially the same life expectancy as uninfected individuals. Also, there is effective pre-exposure prophylaxes which prevents infection from happening in high risk individuals. These advances are real triumphs considering where we were almost 40 years ago but also the reason why it is unconscionable that we leave anyone behind.
As we mark yet again another world AIDS day this December 1st, there are many reasons to feel hopeful about how far we have come since the beginning of the HIV/AIDS epidemic. We have effective treatments that allow people infected with HIV to live normal lives and have essentially the same life expectancy as uninfected individuals. Also, there is effective pre-exposure prophylaxes which prevents infection from happening in high risk individuals. These advances are real triumphs considering where we were almost 40 years ago but also the reason why it is unconscionable that we leave anyone behind.


 Buried amidst the chaos is the ever-present street “pharmacist”. Usually, a small makeshift stand or sometimes just a carton box packed with contraband medicines for all ailments. The stand is typically manned by an ordinary looking person everyone calls “docta”. Projecting an air of confidence on all things health-related next to signs displaying his or her areas of specialty. People stop by for consultations and prescriptions, a quick exchange of cash is made and they walk away with a supply of pills for whatever illnesses they seek to address.
Buried amidst the chaos is the ever-present street “pharmacist”. Usually, a small makeshift stand or sometimes just a carton box packed with contraband medicines for all ailments. The stand is typically manned by an ordinary looking person everyone calls “docta”. Projecting an air of confidence on all things health-related next to signs displaying his or her areas of specialty. People stop by for consultations and prescriptions, a quick exchange of cash is made and they walk away with a supply of pills for whatever illnesses they seek to address.

 Hardly a day goes by without a headline or an article on the opioid crisis that’s sweeping across the US, now considered to be one of the biggest public health crises facing the country. The United States, is one of the wealthiest and most powerful countries in the world, yet
Hardly a day goes by without a headline or an article on the opioid crisis that’s sweeping across the US, now considered to be one of the biggest public health crises facing the country. The United States, is one of the wealthiest and most powerful countries in the world, yet 



 Over the 200 years that followed, his innovation underwent medical and technological changes eventually resulting in the eradication of
Over the 200 years that followed, his innovation underwent medical and technological changes eventually resulting in the eradication of 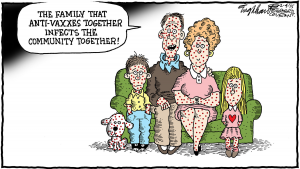 While there is a lot of fear that anti-vaxxers may influence the public view on vaccination and drive the decrease in vaccination uptake, a closer look reveals the problem to be way more complex. T
While there is a lot of fear that anti-vaxxers may influence the public view on vaccination and drive the decrease in vaccination uptake, a closer look reveals the problem to be way more complex. T
 This is the dangerous complacency that puts us all at risk of large outbreaks and losing the ground that we have made with the vaccine revolution. Last year’s flu season, by CDC estimates, was the worst in almost a decade, breaking records just like this year’s measles crisis across Europe. Ultimately we have come too far and should know better than to ignore our most potent tools to fight infection. This message may sound trite but is still as valuable and important today as it was 50 years ago, vaccines prevent disease and save lives. Ignoring that simple fact makes us all less safe!
This is the dangerous complacency that puts us all at risk of large outbreaks and losing the ground that we have made with the vaccine revolution. Last year’s flu season, by CDC estimates, was the worst in almost a decade, breaking records just like this year’s measles crisis across Europe. Ultimately we have come too far and should know better than to ignore our most potent tools to fight infection. This message may sound trite but is still as valuable and important today as it was 50 years ago, vaccines prevent disease and save lives. Ignoring that simple fact makes us all less safe!